Stay Up to Date
Submit your email address to receive the latest industry and Aerospace America news.
Manufacturing licenses coming soon
Early in March, David Van Buren, a flight projects engineer at NASA’s Jet Propulsion Laboratory in Pasadena, California, was growing concerned about projections of global ventilator shortages for severely sick COVID-19 patients. His idea: Put the lab’s engineers to work on designing prototype ventilators that manufacturers could then mass produce quickly for the hospitals that would need them as the number of their coronavirus patients climbed.
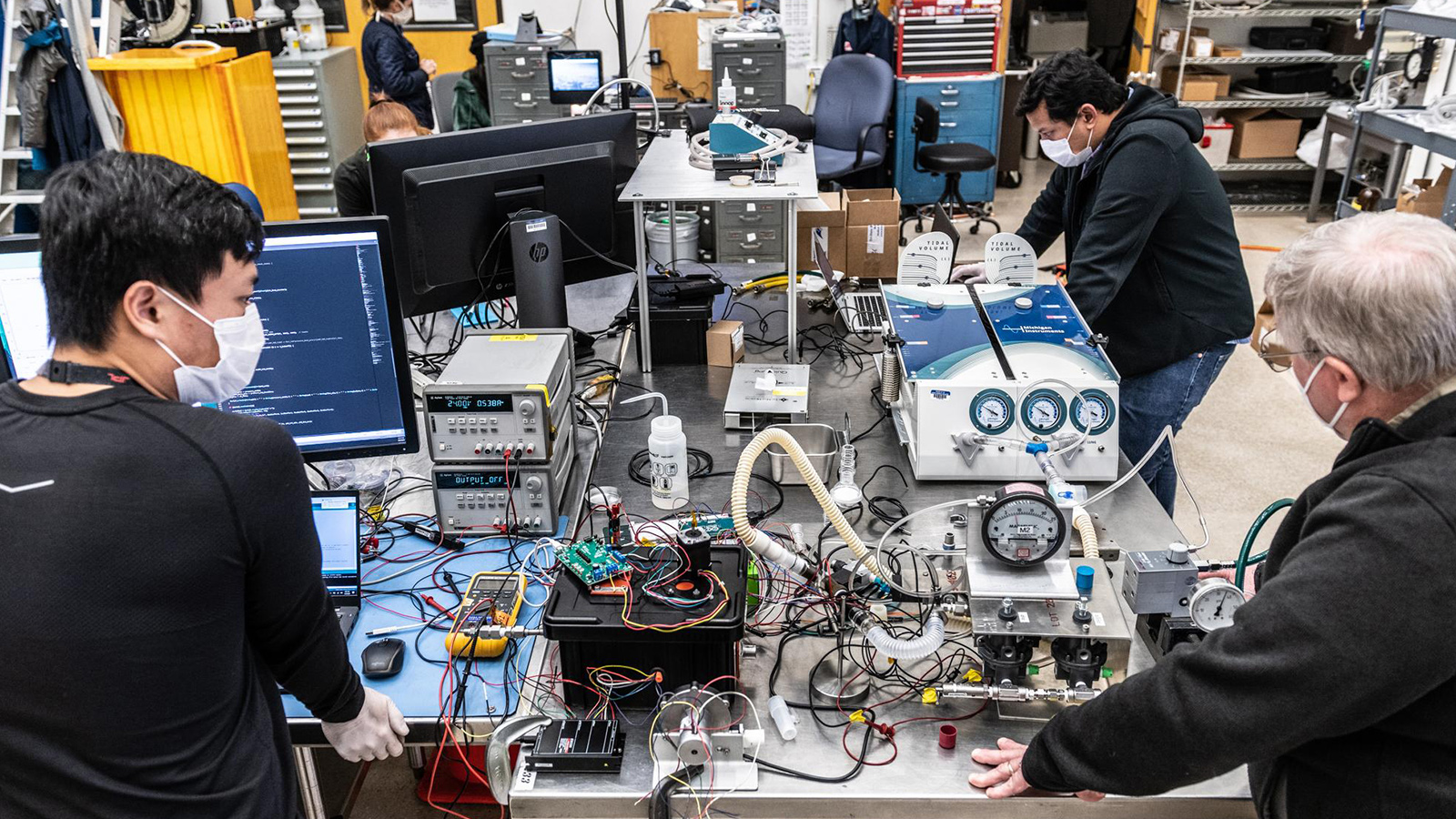
The lab’s chief engineer, Rob Manning, signed off on the idea and within a few days — on March 16 — Van Buren explained the concept to co-workers at the Left Field design bay, so named for the far-out spacecraft ideas that engineers have shared over the years on the room’s white boards. In 35 days, the team finished building the first of two prototypes and two days later it was at the Icahn School of Medicine adjacent to Mount Sinai hospital in New York City for testing. The prototype was hand-delivered there via a commercial flight, giving it its own seat.
The U.S. Food and Drug Administration approved the design on April 30 for emergency use. About 100 manufacturers around the world have now asked to license the design at no charge from Caltech, which operates JPL for NASA. As of late May, engineers from the design teams were evaluating and scoring the license applications and meeting virtually with applicants in 30-minute sessions to answer questions.
FDA approval of a second prototype is pending.
As the 100 or so engineers gathered in March at the Left Field bay, the task brought to mind a certain TV character known for escaping jams with just his wits and duct tape. “As you might imagine, the term ‘MacGyver’ came up,” says Michael Johnson, an electro-mechanical engineer at the lab and chief engineer for the ventilator design team.
They decided to write up a set of requirements, just as they would when starting an aerospace project. They sought out a pulmonologist at Huntington Hospital in Pasadena to teach them what a ventilator for a COVID-19 patient would have to do. The basic idea of a ventilator is simple: It channels compressed air supplied by an outside source or by its own fan turbine into the lungs and then opens a valve to let the lungs push the air out. Before the tutorial, the engineers figured that the task would be akin to figuring out how to rhythmically inflate and deflate a balloon. But then the doctor explained the problems that sick lungs present, such as over-inflation that can occur in a patient over time when the ventilator repeatedly fails to allow the lungs to breathe out fully, a problem called breath stacking. At that point, Johnson says, the engineers looked each other with a new realization: “We know nothing.”
From the doctor’s tutorial and subsequent consultations with other doctors at Huntington Hospital and Santa Monica College, the engineers set the critical parameters that their ventilators would need to maintain for COVID-19 patients. To avoid breath stacking, for example, the engineers designed flow and pressure regulators and sensors to maintain the correct lung pressure and breath intervals as set on the machine by a health care provider. Alarms would be triggered by certain pressure, flow or interval readings.
To keep the designs as simple as possible, they wouldn’t try to build ventilators that could handle a range of sicknesses, like most commercial ventilators do. “If we can make them simple and low-cost enough, then there could be a whole lot more of them, easier and quicker” to build, Johnson says. Also, their ventilators couldn’t have any of the same parts that other ventilators had, or else they would just siphon off the supply chains of others and wouldn’t contribute a net addition to the global population of ventilators.
Once they had set up their requirements, the engineers brainstormed and came up with as many initial designs as they could, just as they would with a new aerospace project. Their goal was to carry as many designs as possible to the prototype stage because more viable designs would mean more opportunities to increase the overall supply of ventilators for the pandemic. At this point, the engineers resisted any urge to look at existing ventilators, because they wanted to come up with designs while being completely blind to how anyone else would do it, Johnson says. “That has benefits in that you don’t get poisoned in your thinking.”
They started with four designs for their VITAL prototypes, short for Ventilator Intervention Technology Accessible Locally. They quickly narrowed the field to two: the VITAL Pneumatic (the prototype built in 35 days) plugs into the pressurized air lines in hospitals. The other design, called the VITAL Compressor, supplies its own pressurized air for situations when air lines are not available, such as in tent hospitals. VITAL Compressor’s prototype was completed in May and a digital file of its design — containing nearly 800 pages of drawings, schematics, instructions for use, photos, data and analysis — was sent to FDA in Washington, D.C., for approval. Other than electronics, the two designs share none of the same parts, so they won’t cannibalize each other’s supply chain. Sharing electronics seemed reasonable because “making a few hundred thousand of something is low-quantity” for electronics manufacturers, Johnson says.
Once the engineers had settled on their designs for these two prototypes, they looked at how existing ventilators were built and were struck by the number of parts in a typical machine: 3,000 to 4,000, compared to fewer than 100 for either of the VITAL designs. They had succeeded at keeping their designs as simple and cheap as possible.
Next, the engineers had to physically build their designs in the brassboard stage by assembling parts end-to-end in a line on a bench to see if they worked before packaging them in a box for the prototype stage. By the second day of the project, the engineers were buying parts, and by the fifth day they had assembled parts on a bench to operate with an artificial test lung they had borrowed from Santa Monica College that had used it for respiratory therapy training.
As the engineers added parts to the brassboard, they learned from talking to the parts vendors that some parts wouldn’t be available in large quantities — tens of thousands — for mass production, so they switched them out for parts that would be available in the quantities needed.
The engineers needed to make sure the two ventilators would work well with the doctors and nurses who would be using them. So they sought their advice, inviting doctors into the lab five or six times and holding a daylong web conference with 60 to 80 doctors, nurses and ICU specialists. They tested their first prototype, VITAL Pneumatic, with the Icahn School of Medicine. They also worked with FDA officials starting on the second day of the project to make sure the designs would meet the agency’s requirements. Just before the engineers built the first prototype, they invited a doctor to the lab to see if he could operate the control panel shared by VITAL Pneumatic and VITAL Compressor. When the doctor walked up to the panel and intuitively figured out how to make an adjustment, without any instructions, the engineers cheered. “We were all jumping up and down and yelling ‘Yeah!’” Johnson says.
The next step was to install the components into boxes to create the prototypes. At this stage, they encountered a new enemy, especially for the VITAL Compressor: heat. Because the ventilators can be called upon to deliver 100% oxygen to some patients, the engineers had to make sure nothing got hot enough to produce an ignition hazard.
The heat issue with the VITAL Compressor surprised the team, given that its design looked much simpler than the pneumatic design. “We thought: ‘Oh, this is going to be so much easier to put together; it will go quicker; this is going to be better in every way,’” Johnson says. But VITAL Compressor was “a thermal nightmare,” mainly because of heat generated by the motors that compressed the air. Their first attempt at a prototype produced air for breathing that was hair-dryer hot.
Because time was of the essence, the engineers decided to forgo their normal process, which would have been to create a detailed model with a step-by-step analysis to zero in on the most likely factors contributing to the heat problem. Instead, they solved the heat issue by making every thermal design change they could think of, all at the same time: adding fans to vents to move air through the housing, changing the motor mounting so heat was pulled out of it more directly, sealing off the air around the motor from the air that is pumped to the patient, adding a muffler that provided some cooling and modulating the current to a solenoid.
The team also wasn’t too proud to seek advice about how to safely pump medical oxygen. They turned to Jonathan Tylka, an expert on medical equipment testing at NASA’s White Sands Test Facility in New Mexico, about the potential ignition hazards posed by overheating or other factors as the ventilators did their pumping. The engineers were familiar with the hazards of managing oxygen stored at 2,000 to 5,000 pounds per square inch for rocket propulsion, whereas medical oxygen typically flows at 0.5 to 1 psi. “That’s a case where our aerospace experience actually worked against us,” Johnson says. “We had to learn in fact the opposite: At low pressures, it’s not quite as dangerous.”
The team had averted some challenges and met others. The task, overall, was not as simple as they thought, and the next step will be to hear that their handiwork is indeed saving lives. “It’s possible to find a team here who can do just about anything. After all, our team can drop little RC [remotely controlled] cars on Mars and drive around and do geology,” says Van Buren.
About Keith Button
Keith has written for C4ISR Journal and Hedge Fund Alert, where he broke news of the 2007 Bear Stearns hedge fund blowup that kicked off the global credit crisis. He is based in New York.
Related Posts
Stay Up to Date
Submit your email address to receive the latest industry and Aerospace America news.