Stay Up to Date
Submit your email address to receive the latest industry and Aerospace America news.
Gene therapy could one day make it possible to biologically enhance humans to live and work in deep space. Adam Hadhazy checks in on this nascent idea.
It’s fitting that many cultures place gods in the heavens above, for living beyond Earth does indeed require a degree of supernaturality.
Spacecraft technology can supply the basics: food, air, water and shelter. Yet during their record-setting, yearlong stays on space stations, astronauts and cosmonauts have dealt with myriad health problems due to exposure to weightlessness and radiation. These brave explorers have not suffered, it seems, any serious, lasting deficits. Those embarking on longer-duration missions outside of the relative protection of low Earth orbit, and thus out past our planet’s radiation-diverting magnetosphere, would likely have greater damage inflicted. Current countermeasures such as exercise, diet and radiation shielding could fall far short in keeping astronauts healthily productive on extended expeditions to the moon, Mars and destinations unbound.
A radical-sounding solution, now gaining traction in academia, is biologically enhancing people for space travel. Increasingly feasible due to galloping advances in medicine and biotechnology, this enhancement would involve altering genes to render would-be astronauts more robust against the ravages of space. The genes could, for instance, make bones superhumanly strong, or ramp up the repairing of DNA strands sundered by radiation.
If one coldly analyzes the hazards of life beyond the magnetosphere, manipulating genes could be the only way. “The idea of human enhancement should be considered by mission planners as a reasonable option,” says Konrad Szocik, an assistant professor of philosophy who studies the topic at the University of Information Technology and Management in Rzeszow, Poland.
The concept is not so far-fetched. After decades of halting progress, gene therapy — the modification of DNA in cells to treat or prevent disease — has arrived. The very first gene therapy approved by the U.S. Food and Drug Administration, for a type of advanced cancer, went on the market in 2017. Hundreds more gene therapies are in clinical trials. “It’s regular medicine,” says Harvard University’s George Church, a pioneer in human genetic engineering.
Nevertheless, gene therapy is still too new for NASA or other space agencies to fund research for, let alone consider adopting the technique. Before changing the genes of someone shot off into space, the therapies must accumulate a substantial record of safety and efficacy terrestrially. Gene therapy is “definitely on our radar, but it’s so immature,” says Jennifer Fogarty, the chief scientist of NASA’s Human Research Program. “We’re cautiously optimistic.”
Genethics
At first blush, gene therapy’s scientific argument looks overshadowed by its gnarly ethical implications, such as the propriety of introducing desirable traits to the human population through eugenics or creating “designer babies.” Those concerns could be managed as follows: The genetic changes for astronauts, as well as most Earthly patients, would not be to the germline cells of sperm and egg, and so the effects would not be heritable. Instead, the modifications would be to DNA in the body’s somatic cells, comprising all other cell and tissue types. In this way, gene therapies intended for astronauts arguably would be little different from today’s conventional drugs and treatments.
Prominent biologists, some of whom work closely with NASA, are furthering the case for enhancement, not just from a scientific basis but also from an ethical one. “There may come a time when it would be ethically irresponsible to send people out into space without some form of genetic protection if we’re able to do it,” says Christopher Mason, an associate professor of physiology and biophysics at Weill Cornell Medical College in New York City.
Mason says that the ethical arguments about applying genetic engineering to human beings fundamentally changes in the astronaut scenario. “The application is in a different space, literally, for someone going to another planet,” he says.
“In my opinion,” adds Szocik, “there is only one strong objection to human enhancement in space — the risk of failure and negative medical consequences. However, I do not see any reasons to treat seriously other kinds of objections, such as an argument of ‘playing god’ or some kind of limitation of autonomy and freedom.”
In these early days for the concept of enhancement, initial progress is coming largely out of work funded for and focused on identifying genes involved in normal deleterious Earthly experience, such as aging, neurodegeneration and disease. The second step is then to characterize those genes for potential modification, with the bonus that many of those same genes also hold promise for helping out humans engaged in long-duration spaceflight.
Harsh final-frontier living
In terms of why deep space is so hazardous to humans, researchers are now gaining granular knowledge about those impacts, which range from broad metabolic and cellular effects to risks of damage to DNA.
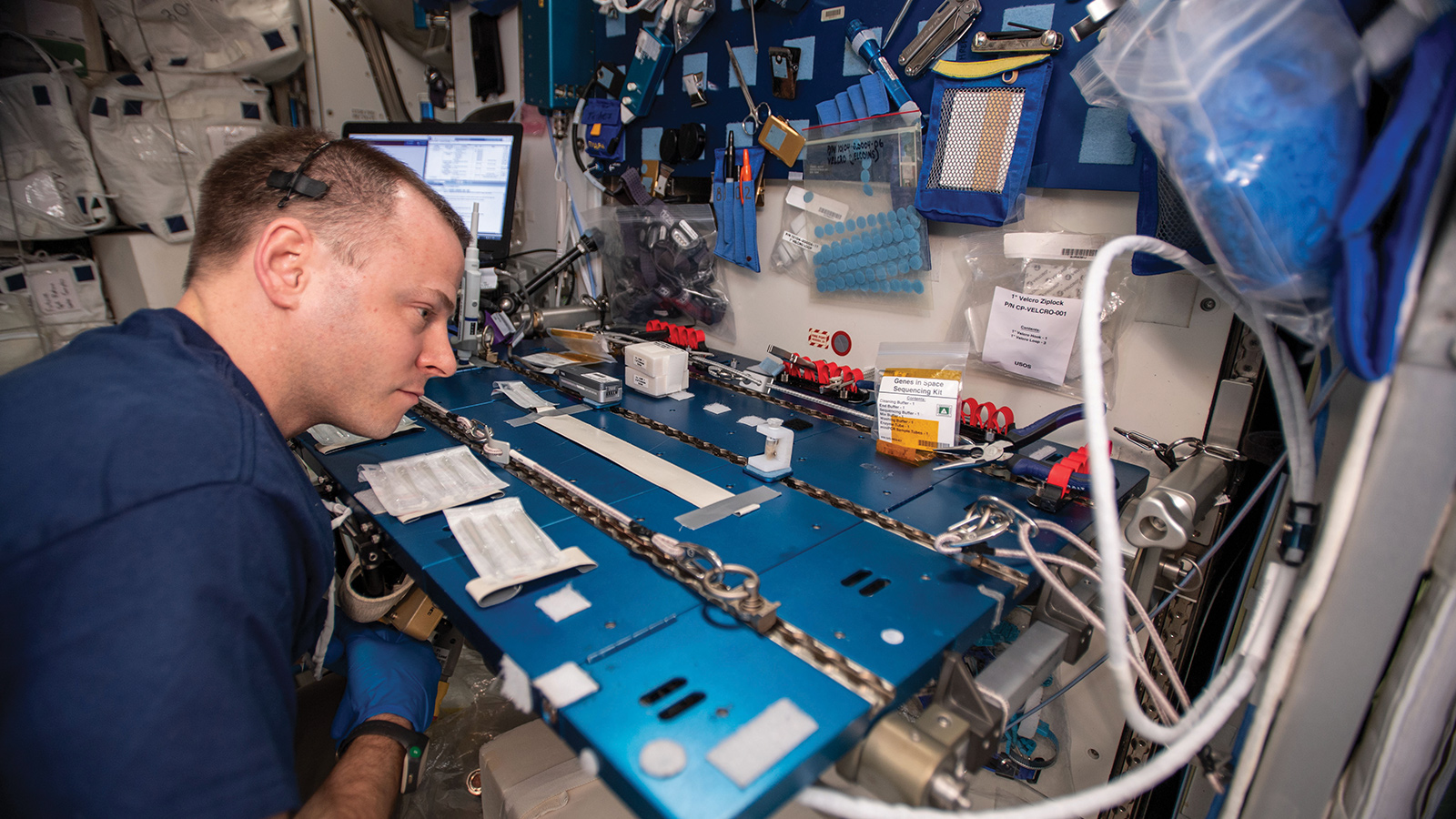
NASA’s Twins Study, which culminated with the release of a paper in the April issue of the journal Science, provides the most comprehensive look yet at the response to weightlessness and radiation. “The study itself was by far the greatest resolution of what happens to the body during spaceflight,” says Mason, a principal author of the study. “We used the entire modern armada of molecular biology and technology.”
The study followed now-retired NASA astronauts Scott Kelly during his March 2015 to March 2016 stay on the International Space Station, and his brother, Mark, who served as a control subject over the same period on Earth. Both Kellys underwent a battery of tests, from blood and urine sampling to gauging their gene expression (activity) levels to psychological and cognitive assessments.
The Twins Study confirmed with sharper precision much of what the hundreds of prior astronaut deployments have documented. The most concerning ailments include muscle atrophy, bone deterioration, weight loss and bodily fluid redistribution.
Physiologists expect that astronauts going farther afield and for longer will fare worse. Barring breakthroughs in propulsion, a roundtrip Mars mission would last over a year. Mason says the voyage would subject astronauts to roughly eight times the radiation dose Scott Kelly received during his year in low Earth orbit. “It’s more,” says Mason, “but not crazy high amounts more,” suggesting countermeasures of some sort could be in reach. Daily exercise, now standard on ISS stays, slows bone and muscle loss from weightlessness but cannot compensate fully. An osteoporosis drug is standard issue on orbit as well, though again, pills won’t be a magic bullet.
“Pharmacology can only take you so far,” says Mason. “To some degree, we need our biology to fundamentally be adapted to space.”
Genetic switches to throw
Toward this end, Harvard’s Church co-founded the Consortium for Space Genetics in 2016. The consortium aims to bring about better living here on Earth, setting the stage for eventual off-planet living. Church and his colleagues have identified a few dozen genes that hold promise, covering a gamut of desirable traits for astronautical life. These range from needing less sleep to growing tougher bones, high altitude (low oxygen) adaptions, larger and leaner muscles, reduced pain sensitivity, and transmissible and nontransmissible disease resistance.
Robust mental health is another aim. An example is a gene associated with low rates of bipolar disorder and higher cognitive test performance. Other genes seem to decrease anxiety levels, boost memory and improve spatial learning abilities. If these traits jibe with the declines tied to growing old on Earth, that’s no accident; living in space is comparable to aging in overdrive.
“Radiation can accelerate aging, and low gravity can accelerate osteoporosis,” says Church. “A lot of what my lab works on, besides space genetics, is aging reversal via gene therapy, and those are related topics.”
Church’s hope is that the terrestrial demand for gene therapies to ease aging and potentially treat neurodegenerative diseases such as Alzheimer’s will be the impetus for having therapies approved that could also benefit astronauts.
Meanwhile, Mason, who is affiliated with the consortium, is conducting in vitro studies of human cells in the lab to see how they function with enhanced genetics. A prime example: the repair gene designated p53, located in cells throughout our body. When DNA damage occurs in a cell, p53 cranks out its associated protein, which triggers either repair or, if the DNA’s too far gone, initiates a cell’s self-destruct mechanism. In this way, p53 works as a tumor suppressor gene, heading off potential neoplasms that emerge from botched DNA repair jobs. People with only a single functioning copy of p53 in their genome often develop multiple cancers, and often in childhood.
That’s in contrast to elephants, which possess 20 copies and hardly ever develop cancer — all the more remarkable given these pachyderms’ vastly greater cell count, which presents more opportunities for accumulating genetic errors that lead to malignancies. If sprinkled liberally into astronaut genomes, p53 could augment DNA repair from cosmic radiation damage.
Mason’s investigations also go beyond the realm of human genetics entirely, looking to animals for evolutionary innovations. For example, Dsup, short for “damage suppressor,” is the genetic ace up the sleeve of tardigrades, the astoundingly robust microscopic critters popularly known as water bears. These eight-legged animals can survive all manner of extreme conditions, including high and low temperatures and pressures, starvation and desiccation, plus exposure to a vacuum and radiation. Dsup suppresses breakages in the rungs of the molecule’s double helical ladderlike structure, helping tardigrades famously withstand environmental stressors. If Dsup can be made to get along with human genetics, it could be quite the fortifier.
Still another approach, proposed by Columbia University systems biology professor Harris Wang, calls for genetically modifying human kidneys to manufacture the nine “essential” amino acids. Unlike the other amino acids our bodies require for building proteins, these nine cannot be generated inside our cells, so they must be obtained from food sources. Instead of dedicating tons of spacecraft mass and precious volume for said food supplies, astronauts enhanced in this way could drink sugar water for sustenance. Mason likes the concept.
“The perfect complement to increasing [astronaut] defensive capability” through DNA damage-resistance genes, says Mason, “is to increase survivability and independence from needing anything else.”
From the lab to the clinic
Gene therapy is in use today to treat certain cancers and eye disease, and the treatments are administered intravenously or through an injection. In one method, doctors harvest cells from a patient and genetically modify them to create specific proteins or suppress protein creation, whatever the treatment requires. These engineered cells are then returned to the body where they replicate as usual, engendering a line of cells programmed for specific tasks. In another method, doctors tailor viruses to insert genes into the patient’s genome. Both these mechanisms are part of FDA-approved gene therapies.
Over the past decade, a highly efficient way of gene editing, called CRISPR-Cas9, has taken the field by storm. “It’s a dramatic shift,” says Mason, “and a very welcome one.” An enzyme, Cas9, zeroes in on particular sequences of DNA called CRISPRs (clustered regularly interspaced short palindromic repeats) that can be introduced into genomes, bracketing a particular gene. The whole gene can be cut out, scissorlike, or modified with precision. The first human trials with CRISPR in the United States, for relapsing cancers, got underway in April. China has done most of the human CRISPR work to date, though in 2018 scandal erupted from the apparently unsanctioned editing by a Chinese scientist of embryos to confer resistance to HIV infection. These “CRISPR babies” have provoked calls for a formal moratorium on all germline engineering.
As promising as CRISPR is, ethicists say an abundance of caution must still be taken. CRISPR and other gene editing techniques can have off-target effects, splicing up a genome in unintended locations with potentially lethal impacts. Furthermore, individual genes rarely work in isolation. In most cases, they do not act as simple on/off switches for a single, discrete trait. Instead, genes interact complexly with each other and environmental exposures. Accordingly, boosting (upregulating) — or knocking out (downregulating) a gene to prevent bad function X can instead cause bad function Y — an unintended consequence that may not reveal itself until years after treatment, or only in certain individuals.
“Upregulating a DNA repair gene — like going the p53 route — is very practical,” says NASA’s Fogarty. “But is that the only thing p53 does? Likely not. If you’re going to upregulate, you need to be very mindful of the other roles it plays.”
Tomorrow’s astronauts
When might any of this come to pass? From gene target to therapy, clinical studies demonstrating safety and efficacy necessary for FDA approval usually take eight to 10 years. For serious diseases with few or no other treatments, regulators can approve expedited trials, and the genes in question — say, for thwarting the neurodegeneration of Alzheimer’s — could extend to astronauts. Church is therefore quite bullish on gene therapy, even eyeing it for the first crewed missions to Mars that NASA has talked about launching as soon as the 2030s. “We’ll work hard to try to get it [ready] in time,” he says.
Fogarty suggests that gene therapy’s first use in astronauts might not be as preventative medicine, but rather as treatment after arriving back home from a grueling long-duration mission. This strategy would avoid the risks of unexpected effects from fledgling gene therapies, especially which might only manifest in the uniquely health-stressing environment of space.
On the ethics of adjusting an astronaut’s genes, Mason points out that the engineering would be reversible. “When astronauts come back to Earth, we won’t just say ‘sorry you’re mutated,’” says Mason. “We can reprogram things back the way they were before.”
Mason argues that the bold step of genetic enhancement to ensure human durability, and thus accessibility to space, is not just a matter of scratching the itch for exploration, or scaling up new industries and economies. Instead, it’s a matter of survival of Homo sapiens, enabling us to colonize new worlds or live off-world, permanently. Right now, all of humanity’s eggs, so to speak, are in one planetary basket; the same goes for all life we know of in existence.
“We have a duty not only to our species,” says Mason, “but everything else on Earth.”
“Pharmacology can only take you so far. … To some degree, we need our biology to fundamentally be adapted to space.”
Christopher Mason, Weill Cornell Medical College, New York City
About Adam Hadhazy
Adam writes about astrophysics and technology. His work has appeared in Discover and New Scientist magazines.
Related Posts
Stay Up to Date
Submit your email address to receive the latest industry and Aerospace America news.